Introduction
The risk adjustment (RA) program for health plans participating in Affordable Care Act (ACA) state marketplaces is largely based upon prescription drug utilization data and diagnosis codes documented during medical visits associated with plan enrollees. The primary sources of RA information are the encounter submissions that plans make to the External Data Gathering Environment (EDGE) servers (a data collection service that health plans must use to submit enrollee information as well as medical encounters and pharmaceutical claims). As discussed in the first blog of this series, it is possible that these encounter submissions may be missing relevant diagnoses for a health plan member or may have incorrect information. In such cases, a health plan has the option of submitting Supplemental Diagnosis Code (SDCs) files.
SDC submissions have a large impact on a plan’s relative risk score under the ACA RA program, increasing plan risk scores by approximately 10% on average. Consequently, SDCs can also have a meaningful impact on plan RA transfer payments, making it critical for any plan participating in an ACA marketplace to understand the role of SDCs. We previously provided more details on what SDCs are and how they are submitted for consideration in the ACA risk adjustment process. In this blog, we revisit some of the analyses already presented using 2018 data, this time also including 2019 data from the EDGE Limited Data Set (LDS) (The EDGE LDS contains de-identified enrollment and encounter data that is derived from the data collected and used for the ACA RA program). Looking at multiple years can help us gain insights on the consistency of trends in SDC submissions and their impacts. In general, we find that the pattern of SDCs is very consistent over time, underscoring the importance of health plans understanding the role of SDCs in their RA processes and the transfer payment calculations.
Number of HCCs Impacted by SDCs Each Year
According to data from benefit year 2018, the submitted supplemental diagnosis information would impact 1.4 million Hierarchical Condition Category (HCC) codes. The vast majority (86%) of these HCC codes would be added on by a SDC submission, as opposed to HCC codes being deleted. There were even more HCCs impacted for benefit year 2019 (1.5 million), with a similar percentage (86%) being additions due to a SDC submission.
Exhibit. Number of HCCs Impacted by the SDC submissions
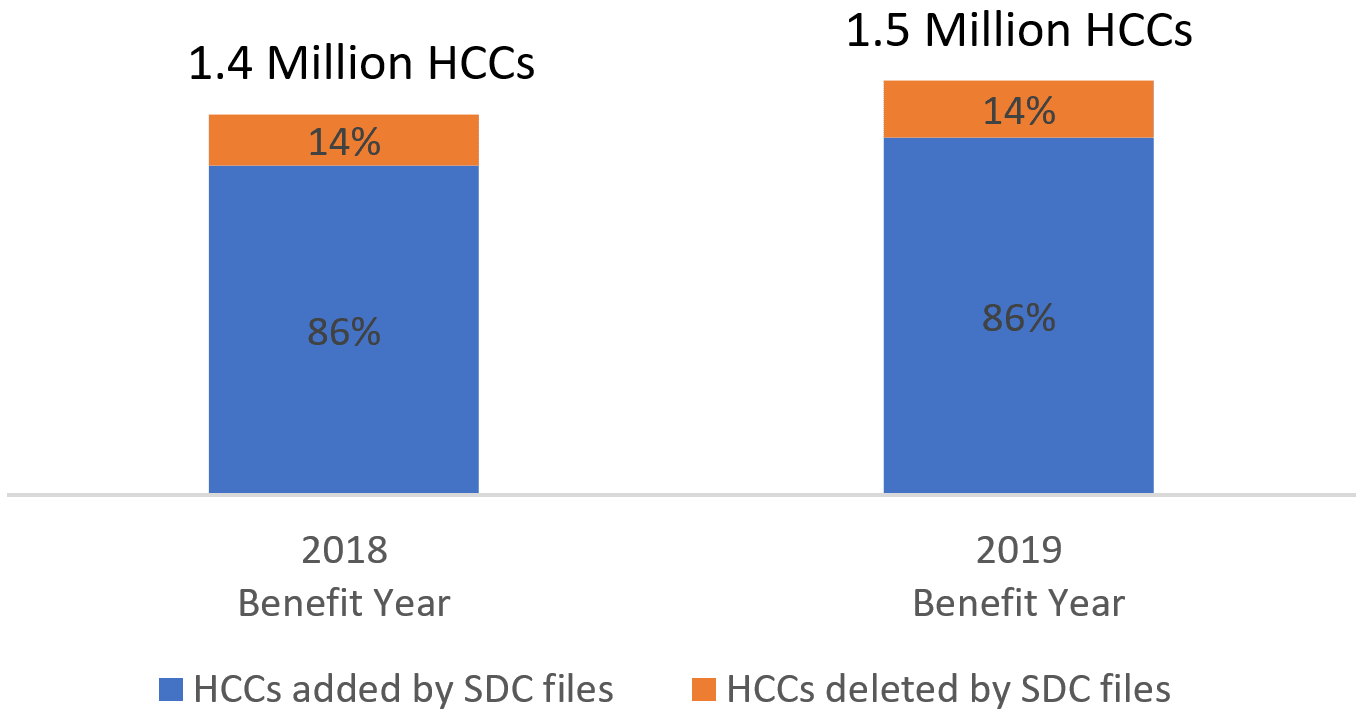
Source: RaLytics, LLC analysis of the 2018 and 2019 Enrollee-Level External Data Gathering Environment, Limited Data Sets.
SDC Impact on Plan Risk Scores Each Year
For both benefit year 2018 and 2019, the HCC additions comprise approximately 9% of the total HCCs identified by submitted diagnoses, either through the encounter or supplemental submissions. Because these additions are slightly biased towards diagnoses associated with HCCs having larger risk adjustment factors, the net effect of the additions (after taking into account deletes) to the average plan’s relative risk score would be an approximately 10% increase. The net effect increased slightly in benefit year 2019 compared to 2018 (10.6% compared to 9.9%).
Top HCCs Impacted
Below are the five HCCs associated with the largest change in value due to net additions in SDC submissions for the 2018 benefit year:
- HCC 254: Amputation Status, Lower Limb/Amputation Complications (4.517)
- HCC 251: Stem Cell, Including Bone Marrow, Transplant Status/Complications (25.162)
- HCC 18: Pancreas Transplant Status/Complications (4.599)
- HCC 34: Liver Transplant Status/Complications (11.061)
- HCC 183: Kidney Transplant Status (8.31)
The same HCCs were also in the top five for the 2019 benefit year (although in a different order). These HCCs also generally represent lifelong conditions with relatively large risk adjustment (RA) factor values (the RA factors used in platinum plans during benefit year 2018 are shown in parentheses following the HCC names above). Given the high costs associated with managing the care for members with these conditions, it is imperative that these codes are captured correctly.
Conclusion
In general, it appears from looking at the 2018 and 2019 data, there is a very similar pattern in terms of which HCCs are most impacted by SDC file submissions. (In fact, there is very high correlation—over 0.90—when comparing the ranking of HCCs by most to least impacted by SDC submissions for benefit years 2018 and 2019). Given these consistencies, plans may consider exploring the reasons for high levels of additions or deletes for specific HCCs. Without any intervention, it is likely that similar patterns will persist. Generating lists of HCCs that have had a relatively large impact by the SDC submissions can help target additional training for clinicians on best practices for documenting diagnosis codes on medical records. In addition, these lists can be used to ensure that appropriate levels of disease management are being provided to plan members.
Interested in adding capabilities to ensure that key diagnoses for risk adjusted payments are appropriately documented and identified? Contact RaLytics for more information: info@ralytics.com.
